Osteoarthritis (OA)
Definition
Osteoarthritis (OA) is a disorder of synovial joints characterised by focal degeneration of articular cartilage with irregular regeneration and remodelling of subchondral bone. OA originates from the Greek word "osteo", meaning " bone", "arthro", meaning "joint", and "itis", meaning inflammation, however most patients have little or no inflammation. It is believed that OA is due to wear and tear, as OA typically is not present in younger people. However, while age is associated with OA incidence, there is no causal relationship it merely illustrates that OA is a process that takes time to develop. "Degenerative arthritis" is often used as a synonym for OA, but the latter involves both degenerative and regenerative processes.
Facts
Worldwide, OA is the most common joint disorder it costs 1.1% of GNP and it accounts for half of all Non- Steroidal Anti-Inflammatory Drug prescriptions. In western countries, radiographic evidence of this disease is present in 80 percent of patients by 65 years of age and 60 percent of these are symptomatic. OA is the most common form of arthritis, and the leading cause of chronic disability in Ireland.
Up to one in six people or 750,000 suffer with arthritis in Ireland. It is reported that the lifetime risk of symptomatic knee OA may be nearly one in two, or 46%. However, in the obese nearly two in three adults may develop painful knee OA over their lifetime. Life expectancy is increasing and octogenarians and the population over the age of 65 is predicted to quadruple and increase from 11% to 25% by 2040 respectively. Risk factors for developing OA include age greater than 45 yrs, female gender, obesity and a positive family history.
Aetiology
OA has primary (idiopathic/familial/hereditary) and secondary causes. Genetic causes include mutation of the genes for type II procollagen on Chromosome 12 and Interleukin 8 and Vitamin D receptors.
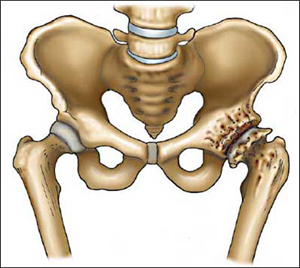
Secondary causes include structural (fracture/instability/previous total meniscectomy –100% experience arthroses by 20 yrs), Congenital/Developmental (developmental dysplasia of the hip, perthes, slipped upper femoral epiphysis), Inflammatory and endocrine (acromegaly, onchronosis, haemochromatosis). In fact between 21 to 48 % of OA of the hip has been linked to dysplasia of the hip. Research has found that young adults with knee injuries have six times the risk of developing osteoarthritis by age 65 compared to adults without knee injuries. For those with hip injuries, the arthritis risk is three times greater.
Other factors that significantly contribute to the development of OA include being overweight (obesity is the strongest risk factor for developing OA of the knee) and occupation (e.g. Osteoarthritis of the hip is particularly common in farmers).
Pathophysiology
Articular cartilage is composed of water, type II collagen (providing tensile strength), proteoglycans (compressive resistance), chondrocytes and other matrix proteins. As type II collagen has a turnover of 360 yrs in adult cartilage it has no capacity for regeneration.
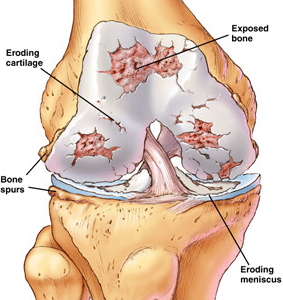
In OA, a variety of potential forces listed above may initiate processes leading to loss of articular or hyaline cartilage -- a strong protein matrix that lubricates (reducing friction) and cushions (load distribution) the joints. On a cellular level OA may be a result of a failed attempt of chondrocytes to repair damaged cartilage which may be mechanical or chemical in origin. In contrast to ageing cartilage, osteoarthritic cartilage has increased water content and proteoglycan degradation. As the body struggles to contain ongoing damage, immune and regrowth process can accelerate damage. When bone surfaces become less well protected by cartilage, subchondral bone may be exposed and damaged, with regrowth leading to a proliferation of ivory-like, dense, reactive bone, a process called eburnation. The patient increasingly experiences pain upon weight bearing, including walking and standing. Due to decreased movement because of the pain, regional muscles may atrophy, and ligaments may become more lax.
Clinical Features and Diagnosis
Presentation
The clinical symptoms of OA may include joint pain, tenderness, stiffness, deformity, swelling and crepitus of joints.
The typical patient with OA is middle-aged or elderly and complains of pain in the knee, hip, hand or spine. Most often, the patient has pain and stiffness in and around the affected joint, along with some limitation of function. The symptoms are often insidious in onset but occasionally may be rapidly progressive. Humid and cold weather increases the pain in many patients.
Pain typically worsens with use of the affected joint and is alleviated with rest. Pain at rest or nocturnal pain is a feature of severe OA and a strong indicator for arthroplasty surgery.
Patients with OA of the hip may complain of problems with gait. Pain can vary greatly in site and nature, which sometimes makes early diagnosis difficult. The pain may be felt in the area of the buttock, groin, thigh or knee, and it can vary in character from a dull ache to a sharp, stabbing pain. Hip stiffness is common, particularly after inactivity, and can be a presenting feature. For example, a patient may mention that a stiff hip makes it difficult to put on shoes and socks or address foot hygiene. Early physical signs of osteoarthritis of the hip include restriction of internal rotation and abduction of the affected hip, with pain occurring at the end of the range of motion. Patients with osteoarthritis of the knee often complain of instability or buckling, especially when they are descending stairs or stepping off curbs.
Examination
The physical examination should include a careful assessment of the affected joints, surrounding soft tissue and bursal areas. The range of movement, contractures, deformities and stability should be noted. Crepitus, which is felt on passive range of motion, is due to the irregularity of opposing cartilage surfaces and is a frequent sign of osteoarthritis of the knee. A complete examination should include assessment of the joint above and below (n.b. referred pain to the knee from the hip) and neurovascular status of the limb. OA generally does not have an inflammatory component, except in advanced disease. The presence of a hot, erythematous, markedly swollen joint suggests a septic joint or a crystal arthropathy such as gout, pseudogout or hydroxyapatite arthritis. OA secondary to a metabolic, genetic or other joint disorder should be suspected in the patient with widespread disease, a prominent inflammatory component, an unusual joint distribution or disease onset before 50 years of age.
Radiographic Features
Diagnosis is normally done through x-rays. It is vital that appropriate weight bearing x-rays are taken of the affected joint in two orthogonal views. The cardinal radiographic features of the disease are subchondral ("below cartilage") sclerosis, subchondral cysts from synovial fluid entering small microfractures under pressure, narrowing of the joint space between the articulating bones, and bone spur formation (osteophytes). Other useful diagnostic techniques include MRI (magnetic resonance imaging), CT , Bone scans, arthrocentesis, joint injection and arthroscopy. However, diagnosis can usually be made by a careful study of the duration, location, the character of the joint symptoms, and the appearance of the joints themselves. The association between joint pain and the radiographic features of OA is not constant, in that many joints with pathologic or radiographic evidence of this disease remain asymptomatic. Equally minimal radiographic changes may be present in patients with moderate to severe pain.”treat the patient not the x-rays” and “beware the normal x-ray”.
Treatment- Conservative vs Operative
Generally speaking, the process of clinically detectable OA is irreversible and can not be cured by non-surgical means. Typical treatment consists of medication or other interventions that can reduce the pain of OA and thereby improve the function of the joint. The Mayo clinic recommends that patients should attend their General Practitioner if they have suffered with swelling, pain or stiffness for greater than two weeks. Early referral to a specialist is also valuable as it allows for early decision for treatment, access to specialist investigations and diagnostic injections. Anecdotally patients suffering pain on a daily basis, requiring analgesia, who struggle to walk a mile and perform activities of daily living and in particular have night pain should be considered for arthroplasty surgery. “do not suffer in silence”
However, the treatment of OA should be individualized. Medical co morbidities such as cardiac disease, hypertension, peptic ulcer disease or renal disease must be considered, and the patient's needs and expectations should also be taken into account.
Conservative
- Conservative
- Analgesia/anti-inflammatories
- Weight loss
- Physiotherapy
- Walking aids
- Occupational aids
- Alternative therapies
Nonpharmacologic Management
No matter the severity or location of OA, conservative measures such as weight control, appropriate rest and exercise, and the use of mechanical support devices are usually beneficial.
Patient Education. . Proper advice and guidance by a health care provider is important in OA management, enabling people with this condition to improve their quality of life. Participation in such courses has been associated with decreased pain and improved quality of life.
Exercise. Patients are often concerned that joint use will "wear out" a damaged joint. However, the available evidence shows that regular low-impact exercise in OA joints does not increase the development of OA.
The goals of an exercise program are to maintain range of motion, muscle strength and general health. All patients with osteoarthritis of the knee should be taught quadriceps-strengthening exercises and should be encouraged to perform them every day. Applying local heat before, and cold packs after exercise, can help relieve pain and inflammation, as can relaxation techniques.
Assistive Devices. In OA of the knees, knee braces, a cane, or a walker can be helpful for walking and support. The use of an appropriately selected cane can reduce hip loading by 20 to 30 percent. The top of the cane's handle should reach the patient's proximal wrist crease when the patient is standing with arms at the side. The cane is usually held on the unaffected side of the body.
Physiotherapy/Occupational therapy. Patients with specific physical disabilities may benefit from physical and occupational therapy. The physical therapist can provide an individualized exercise program and teach the patient how to use therapeutic heat and massage. An occupational therapist can determine whether the patient needs assistive devices such as a raised toilet seat, sock aids etc.
Weight Management. There is a longitudinal association between obesity and OA of the knee in men and women, although obesity is a greater risk factor in women. Therefore, primary preventive strategies may include measures to avoid weight gain, or to achieve weight loss in overweight patients. Further studies are needed to determine if weight loss has a role in the tertiary prevention of osteoarthritis. Up to 6-8 x body weight in force can occur across the patellofemoral articulation in certain activities i.e stair climbing/deep squats.
Pharmacologic Treatments
Supplements
Some have widely proclaimed dietary supplements such as glucosamine sulphate and chondroitin sulphate to be "cures" for arthritis. However, “the jury is still out”, as two studies have been performed one in favour and one discounting glucosamine as an effective treatment. Further research in the form of randomized controlled trials are are required to determine whether glucosamine sulphate and chondroitin sulphate are safe, tolerated and effective in patients with OA.
Simple Analgesics
A large number of medicines are prescribed for and consumed by patients with OA, largely for the relief of pain. The recognition that pain in OA is not necessarily due to inflammation has led to an increased awareness of the role of simple analgesics in the treatment of this disease. A mild analgesic may be sufficiently efficacious. Paracetamol is commonly used to treat the pain from OA.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
In patients requiring NSAID therapy, concurrent use of paracetamol may allow the NSAID dosage to be reduced, thereby limiting toxicity. In the individual patient, cost, dosing frequency and medication tolerance may influence NSAID selection.
If an NSAID is to be used, safety is an important issue, especially in the elderly. The risk of NSAID-induced renal and hepatic toxicity is increased in older patients and in patients with preexisting renal or hepatic insufficiency. Thus, it is important to monitor renal and liver function. Misoprostol, a synthetic prostaglandin E1 analog, and Proton pump inhibitors help to prevent gastric ulcers.
COX-2 selective inhibitors
The presently available NSAIDs work through nonspecific inhibition of cyclo-oxygenase isoforms 1 and 2 (COX-1 and COX-2). COX-1 is expressed in gastric and renal tissues (among others), whereas COX-2 is inducible and is part of the inflammatory response. COX-2 selective inhibitors reduce this risk substantially. These latter NSAIDs carry an elevated risk for cardiovascular disease, and some have now been withdrawn from the market.
Topical treatments are treatments designed for local application and action. There are several NSAIDs available for topical use (e.g. diclofenac, ibuprofen, and ketoprofen) with little, if any, systemic side-effects and at least some therapeutic effect. The more modern NSAID formulations for direct use, containing the drugs in an organic solution or the Transfersome carrier based gel, reportedly, are as effective as oral NSAIDs. Capsaicin (e.g., ArthriCare), a pepper-plant derivative, has been shown to be better than placebo in relieving the pain of OA if applied sufficiently frequently.
Opiates. For moderate to severe pain, narcotic analgesics such as tramadol, and eventually opioids (hydrocodone, oxycodone or morphine) may be necessary. They should be used for short periods to treat exacerbations of pain. These agents are not recommended for prolonged use because they cause constipation and increase the risk of falling, particularly in the elderly.
Intra-Articular Injections.
Corticosteroid. Patients with a painful flare of OA of the knee may benefit from intra-articular injection of a corticosteroid such as triamcinolone or depomedrone. A joint should not be injected more than three or four times in one year because of the possibility of cartilage damage from repeated injections. Patients who require more than three or four injections per year to control symptoms are probably candidates for surgical intervention.
Patients with painful OA of the hip may benefit from intra-articular corticosteroid injections. These injections should be performed under fluoroscopic guidance after arthrogram confirmation and are useful in a diagnostic and therapeutic fashion especially with concomitant back and radicluar pain.
Hyaluronic Acid. Hyaluronic acid is a major nonstructural component of the synovial and cartilage extracellular matrix. It confers viscoelastic and lubricating properties to the joint. In patients with OA, the concentration and the molecular weight of hyaluronic acid are decreased. Thus, viscosupplementation with hyaluronic acid like products is thought to be a possible treatment for OA.
Studies have found that when used as a replacement or an adjunct for NSAID therapy in patients with OA of the knee these injections were at least as effective as continuous NSAID therapy in all outcome measures except activity restriction.
Operative
- Injection
- Arthroscopy
- Arthrodesis
- Excision Arthroplasty
- Osteotomy
- Resculpturing
- Partial Replacements
- Resurfacing
- Total joint replacement
Operative
Patients whose symptoms are not adequately controlled with medical therapy and who have moderate to severe pain and functional impairment are candidates for orthopedic surgery. Injection therapy is useful in patients where other diagnosis need to be excluded and in patients to frail for surgery, for symptom control. Arthrodesis and excision arthroplasty (girdlestones) are now very rarely indicated in patients with primary hip or knee OA. Recent guidelines have suggested that arthroscopy is not indicated in established OA of the knee. Osteotomy may be performed if significant malalignment of the knee or hip joints is present (periacetabular osteotomy in dysplasia) but not with established OA. Resculpturing surgery is a relatively new tool for dealing with Pincer or Cam type impingement of the hip but long term results are awaited. Partial replacements are useful in very specific indications in the knee as either unicondylar or patellofemoral replacements. Resurfacing of the hip is now being performed less often as more stringent indications have been demonstrated. Total joint arthroplasty remains the gold standard of joint arthroplasty and is one of the most successful medical innovations developed during the twentieth century. In fact, in October 2007, The Lancet published a review article entitled "The Operation of the Century: Total Hip Replacement.
Joint replacements have been documented to relieve pain, improve function, correct deformity, increase social mobility, preserve an independent lifestyle, and contribute to psychological well-being. Furthermore, joint replacements are cost-effective medical treatments that provide substantial improvements in quality of life.
Current concepts in Hip and Knee replacement to follow.
Post op Right THR

Pre-op Severe rapidly destructive Osteoarthritis

Hip Osteoarthritis
Knee Osteoarthritis
|

