Hips
Current concepts in total Hip Arthroplasty
Introduction
Total hip arthroplasty (THA) is one of the most successful medical innovations developed during the twentieth century and the results have been well validated and provide substantial improvements in quality of life.
The rate of hip arthroplasty world wide is increasing as a result of an expanding and aging population and the demonstrated clinical success of joint replacement. Between 2005 and 2030, the prevalence of primary THA procedures in the United States is expected to increase 174% and the prevalence of revision hip replacements are expected to increase 137%. In Ireland, based on VHI statistics, THA have increased in number by 93% between 1999 and 2004.
Arthritic joints are associated with pain, stiffness, reduced function, and limitation of activity. When joint replacements were being developed during the 1960s and 1970s, the primary indication was pain. In 2009, pain continues to be the principal reason patients choose joint replacement. However, patients with painful arthritic joints have become less tolerant of activity limitations and preoperative expectations include a short recovery, little or no postoperative discomfort, no perioperative complications, relief of joint pain, increased joint mobility, improved function, long-term durability of the joint replacement, and no limitations of postoperative activity. These expectations are created by documentation of excellent outcomes of joint replacement, orthopaedic marketing, direct-to-consumer marketing, and information and misinformation on the internet. Patients frequently underestimate the challenges involved in the process of joint replacement and overestimate its outcome.
Recent advances have introduced better bearing materials to reduce wear and greatly increase serviceable life. These new materials have been improved to such a degree that many young and active patients may avoid revision of their prosthesis for the rest of their lives. Better designs have increased stability and function so the implant also feels more natural to the patient.
History
The earliest recorded attempts at THA (Gluck T, 1891) were carried out in Germany and used ivory to replace the femoral head. In 1925, a surgeon in Boston, Smith-Petersen, molded a piece of glass into the shape of a hollow hemisphere which could fit over the ball of the hip joint and provide a new smooth surface for movement. Both these attempts led to early failures.
The very early days of THA centered on the use of metal-on-metal bearings (George McKee of Norwich, England, 1953). These produced widely varying clinical results, due primarily to vagaries in design and manufacturing capabilities. Professor Sir John Charnley was convinced that the metal on metal articulation of the McKee joint was unsatisfactory. This search took him into the field of polymers and his first attempt at THA in the early 1950's used Teflon but met with early failure. Charnley's next attempt at THA began in 1962 and involved a stemmed cemented femoral component, a 22.25 mm femoral head and a high-density polyethylene cup inserted into the acetabulum.
The small (22.25mm) head was used in order to minimize plastic volumetric wear but had two undesirable side effects linear penetration into the polymer cup was increased and stability was compromised.
By the mid-1970’s, metal-on-metal arthroplasty was all but abandoned as Sir John Charnley’s technique for low friction hip arthroplasty, using metal-on-polyethylene bearings, became widely accepted. It is now accepted that a Charnley hip replacement can give perfectly satisfactory results in an elderly inactive population (failure of below 1% per year).
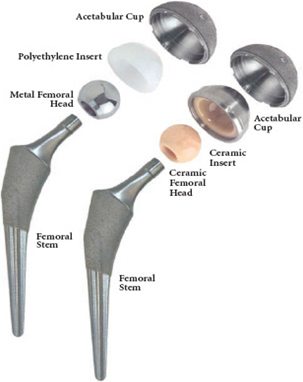
Since the successful operation performed by Sir John Charnley over forty years ago, THA has come a long way. Today there are a multitude of different components, allowing for a variety of options based on a patient’s specific needs.
Fixation
The method of fixation of THA is either with cement or biological fixation of bone to the prosthetic interface. Debate continues as to the optimum femoral stem fixation in THA. Early success in survivorship of cemented stems in THA established a track record that continues to rival that of the most successful cementless stems. Despite this success, however, recognition must be given to the skill and art with which successful cemented technique is performed. In the absence of proper technique, optimal outcomes may fail to be realized. There has been a trend towards uncemented fixation because of reports of higher loosening rates in young active patients. Cemented fixation is static and if microfractures occur with continued cyclical loading the cement cannot remodel. Cement has no endurance limit and will eventually fail. In contrast uncemented fixation is biological (bone ingrowth to porous structure) and dynamic. Concerns with the use of cementless fixation include ingrowth, migration, stress shielding and thigh pain. The introduction of hydroxyapetite coating and a tapered geometry have increased survivorship further. Several types of titanium foam metal have been introduced into clinical application over the past five years. These materials generally have a larger pore structure that promotes greater bone ingrowth as compared with standard beaded or plasma-sprayed titanium surfaces.
The English National Joint Register has shown that cemented hip replacements are on the decline and account for 38% of all cases whereas uncemented hips have increased to 33%. Medium to long term success of top performing femoral prosthesis cemented and uncemented exceed 90% at 15 yrs. The “Achilles heel” of THA is the acetabular component. Porous ingrowth cups may reduce the need for revision of the acetabular component and could potentially allow for exchange of the liner rather than the whole component.
Bearing Options
A traditional THA uses a metal ball of 28 millimeters in diameter and a plastic socket for motion. While it has an excellent record for long life and durability, the plastic wears with each step and can lead to eventual loosening of the hip replacement. In many cases this loosening phenomenon is associated with osteolysis (bone loss), caused by the body’s response to particles of polyethylene debris released from the bearing surface. This process can take between 10 and 20 years. Inevitably, with the younger more active patient group (50% of females 50 yrs of age today may live to 100 years old!), this process is accelerated, potentially leading to earlier failure of the implant and the consequent need for a difficult revision procedure.
Also many older people these days are in good health, live very active lives, and expect to live well into their nineties. Clearly these are “high demand” patients who deserve a high quality THA that will serve them well for the rest of their lives.
Research and advances in tribology have led to bearing surfaces with significantly better wear characteristics. These can broadly be defined as “Hard on Soft” and “Hard on Hard” bearings:
Hard on Soft
- Metal or Ceramic with Conventional Polyethylene Liner
- Metal or Ceramic with Highly Cross Linked Polyethylene
Hard on Hard
- Metal on Metal (MOM) Devices
- Ceramic on Ceramic Devices
Hard on soft
Metal-on-Conventional Polyethylene (Ultra high molecular weight) has been the leading artificial hip component material chosen by surgeons. Polyethylene is the most understood and used of all the liner material and is the least expensive bearing. Metal-on-Polyethylene implants wear at a rate of about 0.1 mm each year.
Ceramic heads are harder than metal, are the most scratch resistant implant material and can greatly reduce the wear rate on the polyethylene bearing. Ceramic-on-Polyethylene implants wear at a rate of about 0.05 millimeters each year, i.e. 50% less than Metal-on-Polyethylene
New wear resistant polyethylene liners have been introduced, called highly cross linked polyethylene. During the manufacturing process the plastic is treated with a short burst of radiation this results in cross-linking and an extremely wear-resistant material. In addition, the data show that these bearing surfaces may have the additional benefit of allowing a much larger diameter bearing surface to be used, which may significantly reduce the likelihood of dislocation. However, the mechanical properties of polyethylene are altered during the cross-linking process. Reduction of material strength and toughness may result in fracture, particularly in very thin components with elevated rims which have been malpositioned. Newer second generation techniques involve annealing rather than melting improving the strength. Vitamin E, a natural antioxidant, stabilized highly cross linked polyethylene bearing material is expected to improve the longevity of the implant bearings used in THA.
The newer, highly cross linked polyethylene liners have shown wear rates as little as 0.01 millimeters each year.
Hard on Hard
Metal on Metal
The ball and socket of the Metal on Metal hip devices are made of Cobalt-Chrome. Advantages of metal-on-metal bearing surfaces include low wear rates, capacity for self-polishing, allow a higher activity level and the possibility for larger/anatomic sized heads (improved range of motion, less dislocation). Investigators have reported excellent survival rates of some first generation metal on metal implants (McKee) when the mechanical couple was exact. The intermediate-term follow-up of metal-on-metal THAs are similar to those seen with metal-on-polyethylene articulation. In addition, given the lack of osteolysis, metal-on-metal articulation may play a role in reducing the wear that occurs with "classic" THA. There have been concerns regarding local and systemic effects of wear debris. Although wear is reduced, the wear products (sub-microscopic particulates, soluble metal ions) are distributed throughout the body. This has raised concerns about long-term bio-compatibility. At present these are only concerns, for there have been no definitive clinical findings that these wear products are harmful with regards to toxicity and carcinogenesis. More studies have been reported with regard to lymphocyte aggregation, ALVAL (aseptic lymphocytic vasculitis-associated lesions) resulting in pseudotumour formation, and metal hypersensitivity. Though this initially was thought to be less than 1% (in men) there may be an incidence of up to 5% in women. One must also be cautious of its use in renal impairment and it should not be used in women of child bearing age.
Metal-on-Metal implants wear at a rate of about 0.001 millimeters each year.
Ceramic-on-ceramic bearings have been in clinical use for nearly forty years. The most significant characteristic of this friction couple is its bioinert nature. In vitro wear studies and retrieval studies have consistently shown alumina–alumina bearings have the lowest wear rate of any available bearing. Further, retrievals of alumina bearings show their resistance to scratching from third body particles. There is a chance of the ceramic components fracturing however improvements in density and grain size have increased the strength of the bearings to the point where the risk is about 1 in 25,000. Concerns with this technology include impingement, locking mechanisms, cost and acoustic phenomena. This squeaking has received much attention recently it is of the order of 1% and it may be related to component malpositioning.
Ceramic-on-Ceramic implants wear at a rate of about 0.0001 millimeters each year.
New Techniques - Computer Assisted Techniques/ MIS/Multimodal analgesia
Computer assisted orthopaedic surgical (CAOS) techniques have been developed to overcome the inherent limitations of mechanical instrumentation. Current computer navigation technologies for total joint surgery use either images ("image-based") or kinematic or surface registration techniques ("image-free") to acquire the anatomic information necessary for guiding surgical procedures. CAOS techniques are being developed to increase the accuracy, reproducibility and a reduction in the number of alignment outliers of a number of steps in THA. They must be safe, accurate, efficient, cost-effective, and adaptable to the various specific THA approaches and instruments. CAOS is also being marketed heavily by the implant manufacturers, though its value remains largely unproven. It accounts for approximately 5% of all cases.
Mini incision surgery (MIS) is the practice of THA by using smaller incisions. MIS is usually best suited for patients with a smaller body mass and seeks to reduce soft tissue damage through reducing the size of the incision. However component positioning accuracy is impaired and surgeons using these approaches are advised to use computer guidance systems. It is important to mention that some orthopedic practices claim that "MIS" is a "minimally invasive procedure" This claim is very false. THA surgery is major surgery, and although in a mini incision case the incision may be smaller, the invasion of the hip capsule remains present. Since the incision is smaller in a mini-incision case, less exposure is achieved, causing for even greater "invasion" in a smaller space. Numerous complications have been associated with MIS including femoral fracture, infection and wound complications, neurovascular injury and malposition. Since MIS is a fairly new practice, no long term data on the success of the operation is available and sustained superior functional outcome following MIS has not been conclusively documented. Patients usually learn about these techniques on promotional web sites, from companies who advertise implants directly to consumers, and from local surgeons claiming to be “the first” to perform a certain operation. It has been claimed that MIS results in faster Recovery and less Discomfort however most of these have been conducted with rapid recovery programmes and new anaesthetic techniques. My philosophy is to do the surgery as safely and as effectively as possible through the smallest incision possible.
Multimodal Analgesia
The concept of pre-emptive analgesia has evolved beyond the importance of reducing the nociceptive afferent input brought about by the surgical incision. The term preventive analgesia was introduced to emphasize the fact that central neuroplasticity is induced by preoperative, intraoperative, and postoperative nociceptive inputs. Multimodal analgesia allows a reduction in the doses of individual drugs for postoperative pain and thus a lower prevalence of opioid-related adverse events. The rationale for this strategy is the achievement of sufficient analgesia due to the additive effects of, or the synergistic effects between, different analgesics. This can be accomplished with the use of nonsteroidal anti-inflammatory drugs, paracetamol, local anesthetics, α-2 agonists (e.g., clonidine), α2 ligands (e.g.,gabapentin and pregabalin), ketamine, and opioids, either alone or in combination. Multimodal analgesia techniques may shorten hospitalization times, improve recovery and function, and decrease healthcare costs following orthopaedic surgery.
Bone conserving hip arthroplasty – Resurfacing/Epiphyseal replacement
The idea of resurfacing the femoral head is really not a new concept. A variety of materials have been tried over the past 100 years, including ivory, gold, plastics and more recently metal. Previous metal-on-metal designs were hampered by tolerancing that resulted in equatorial contact between the femoral and acetabular component articulation, leading to excessively high rates of particle debris and wear.
Design of the hip resurfacing started in 1989 and the first implantation was performed in February of 1991. It is a bone conserving procedure that places a metal cap on the femoral head instead of amputating it. It is therefore more like a natural hip and may allow patients to return to all activities. The ideal candidate for a metal-on-metal hip resurfacing operation is young and active patient that has isolated hip disease with good proximal femoral bone quality and morphology. The theoretical advantages of hip resurfacings include more bone conserving (femur only), improved proprioception, reduced dislocation and easier revision (if only revising the femur). It must be stressed to patients that the surgical exposure is much greater than for a standard hip replacement.
Relative contraindications for hip resurfacing arthroplasty include inflammatory arthritis, severe acetabular dysplasia, poor proximal femoral bone geometry, poor femoral bone stock due to large femoral head cysts, erosive arthritis, a woman of child-bearing age, known metal sensitivities, a limb-length discrepancy of >2 cm and poor renal function. Complications include femoral neck fracture and bone loss, impingement, metal sensitivity issues and the potential for development of ALVAL or pseudotumour formation.
At the present time, it is estimated that hip resurfacing accounts for as many as 6% to 9% of all THA in some countries. There has been intense media coverage as well as frequent postings on patient and industry web sites. The current enthusiasm for hip resurfacing may have led to inaccurate and inappropriate patient expectations. Functional outcomes and gait analysis has not shown significant differences between hip resurfacing and THA. Indeed large metal on metal hip replacements may have a better range of movement due to an improved head neck ratio.
The Australian hip resurfacing registry includes >10,000 hips that have been treated since 1999. The five-year revision rate was 3.8% overall, compared with 2.8% for standard THA. The National Joint Register in England revealed a 5% revision at 3 years and this was much greater in women. These data underscore the importance of patient selection and surgical experience in optimizing the intermediate-term success of hip resurfacing arthroplasty.
Newer devices are being developed and trialed which are cross breeds between resurfacing and THA. These resect more femoral head which means the indications for use may be extended to avascular necrosis, poor femoral bone stock etc. They also load the femoral calcar and may reduce the risk of femoral neck fracture and scalloping (PER).
Conclusions
The relatively early data available regarding alternative bearing surfaces in THA (highly cross-linked polyethylene, ceramic-on-ceramic, and metal-on-metal) are very encouraging. The few implants in which the highly cross-linked polyethylene was used, which were retrieved at revision, demonstrate remarkably little wear, a finding consistent with the corresponding wear-simulator data. Metal-on-metal THA appears to have good clinical results and a very low rate of wear, but high blood levels of cobalt and chromium particles have been detected in patients using these devices. Nevertheless, the toxicological importance and carcinogenic effect of trace metal elevations has not been established and long-term prospective studies are required. Ceramic-on-ceramic bearings appear to be a safe option for young and active patients, demonstrating a very low wear rate and good clinical results. There is lots of conflicting advice in the press and from manufacturing companies. It is therefore important to discuss with patients what type of operative options there are and give informed choice. table 1.
Table 1- Rough guidance:
| Age |
< 55 |
< 65 |
< 65 |
55-70 |
> 70 |
| Men |
Resurfacing
PER |
|
|
Uncemented
MoM/? PER |
Uncemented
MoP |
| Women |
|
Uncemented
CoC/CoP |
Uncemented
MoP |
|
|
PER – Proximal Epiphyseal replacement |
{ As large heads as possible } |
CoC – Ceramic on Ceramic |
| CoP – Ceramic on Highly cross linked polyethylene |
MoM – Metal on Metal (large anatomical heads) |
Modular options with uncemented Total Hip Replacement
Streaming Videos - Hip
|

